Molluscum Contagiosum (MC) is a viral skin infection seen most commonly in young to school-age children. As its name suggests, the MC virus is contagious and spread primarily through direct skin to skin contact, but also by sharing towels, clothing and gym mats. The prevalence of MC seems to be on the rise. A recent meta-analysis suggests a prevalence in children between 5 to 10% with a tendency towards higher rates in 1 to 4-year-olds.¹ There is evidence for increased risk of MC infection in those who have eczema², bathing with an infected sibling, and possibly through swimming pools³, though this should not be a reason to limit swimming.
What does molluscum contagiosum look like?

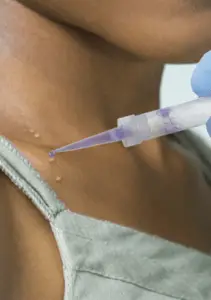
The MC skin infection typically presents as flesh-colored to slightly pink, 1-5mm sized bumps with umbilication (i.e. central depression). Lesions can occur anywhere on the body, but most frequently occur in moist areas of friction including the armpits, groin, elbows, behind the knees, and sides of the abdomen.⁴
MC may also spread to the genital region as well as to the face and eyelids. Bumps often occur in groups, clusters or in a line (from scratching). Fortunately, the MC virus never spreads inside the body.
What are the symptoms of Molluscum Contagiosum?
Many lesions of MC have no symptoms and are usually painless. Other times, lesions may be itchy or irritated and may be surrounded by eczema (“molluscum dermatitis”). Scratching causes MC to spread and multiply. When molluscum lesions turn red in color, it’s usually a good sign that the immune system is starting to clear the infection. If there is no pain or fever, secondary bacterial infection is unlikely.⁵
What happens if I choose not to treat Molluscum Contagiosum?
Most healthy people eventually develop spontaneous immunity against the virus, though it may take months to years to occur. It is impossible to predict how long it will take an individual child (or adult) to develop immunity. If your child has no symptoms, it is reasonable to wait for spontaneous clearance. Since molluscum contagiosum is a “pox” virus, there is a low risk (6-7% chance) of “pock-like” scarring when MC heals⁶.
Some children with MC go on to develop flaring of eczema (molluscum dermatitis), itching, irritation, secondary bacterial infection from scratching, and sometimes an extensive (though benign) rash known as Gianotti Crosti like reaction. And of course, MC can spread to other family and friends until all lesions resolve.
A recently published study (Olsen JR Lancet 2015) states that:
50% of Molluscum Contagiosum lesions resolve spontaneously within 6-12 months
30% of cases persist beyond 18 months
13% of cases persist beyond 24 months

Are there any new treatments available?
Ycanth is the first FDA approved in office treatment for molluscum contagiosum in adult and pediatric patients 2 years of age and older. Ycanth contains the blistering agent cantharidin and produces direct destruction of MC lesions. The liquid is painlessly applied through a special applicator and washed off 24 hours later. Treatments are performed every 3 weeks. Studies show that after three treatments, approximately 50% of patients with MC have complete clearance.

The US Food and Drug Administration (FDA) recently announced its approval of Ligand Pharmaceuticals Incorporated’s Zelsuvmi (berdazimer gel, 10.3%) for the treatment of molluscum contagiosum in patients ages 1 year and older. In the phase 3 study, berdazimer gel demonstrated statistically significant improvements in the clearance of MC lesions. Zelsuvmi is a prescription topical medication that is applied by the patient or family member at home. Unfortunately, Zelsuvmi is not anticipated to be available until the fall of 2024.
Sources
- Fam Pract. 2014 Apr;31(2):130-6. Epidemiology of molluscum contagiosum in children: a systematic review. Olsen JR1, Gallacher J, Piguet V, Francis NA.
- J Am Acad Dermatol. 2006 Jan;54(1):47-54. The epidemiology of molluscum contagiosum in children. Dohil MA1, Lin P, Lee J, Lucky AW, Paller AS, Eichenfield LF.
- Pediatr Dermatol. 2005 Jul-Aug;22(4):287-94. Epidemiology and impact of childhood molluscum contagiosum: a case series and critical review of the literature. She Braue A1, Ross G, Varigos G, Kelly H.
- Pediatr Dermatol. 2009 Jul-Aug;26(4):425-6. Treatment of facial molluscum contagiosum with trichloroacetic acid. Pediatr Dermatol. 2009 Jul-Aug;26(4):425-6. Bard S, Shiman MI, Bellman B, Connelly EA.
- Society of pediatric dermatology molluscum contagiosum parent handout.
- Int J Dermatol. 2006 Feb;45(2):93-9. Childhood molluscum contagiosum. Brown J, Janniger CK, Schwartz RA, Silverberg NB.
- J Am Acad Dermatol. 2000 Sep;43(3):503-7. Childhood molluscum contagiosum: experience with cantharidin therapy in 300 patients. Silverberg NB, Sidbury R, Mancini AJ.
- Pediatr Dermatol. 2007 Mar-Apr;24(2):192-4. Modified curettage technique for molluscum contagiosum. Martín-García RF, García ME, Rosado A.
- Pediatr Dermatol. 2011 May-Jun;28 Intralesional immunotherapy with Candida antigen for the treatment of molluscum contagiosum in children. Enns LL1, Evans MS.