What is Hyperhidrosis?
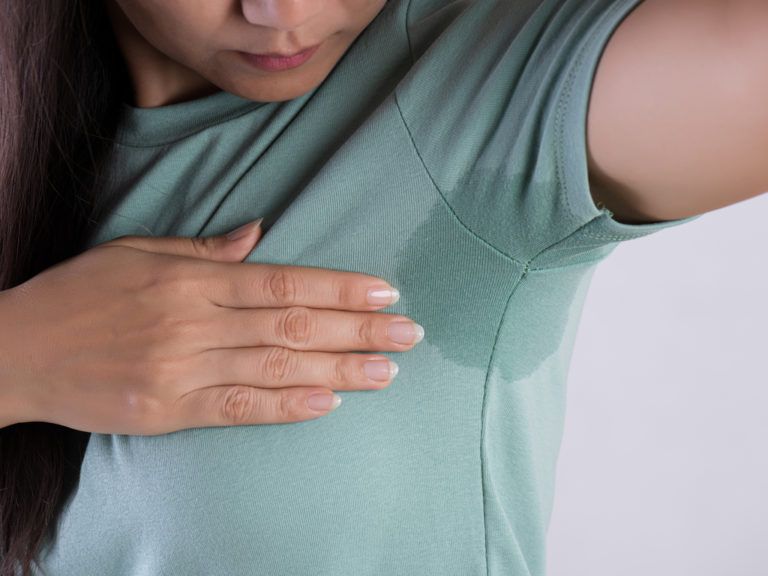
Hyperhydrosis is a disorder characterized by excessive sweat production. Sweating is a normal part of our physiology in order to prevent overheating. Those people who experience hyperhydrosis, however, develop excessive sweating beyond normal needs. The most commonly areas affected are the armpits, palms, soles, face, and scalp ( where sweat glands are most abundant).
Excessive sweating has a negative impact on daily functioning and social interactions, and may lead to depression. Others feel a sense of embarrassment, frustration, insecurity, and avoid social and intimate relationships. Many people who suffer from this condition do not discuss his/her sweating problem with others.
Current data estimates that approximately 5% of the United States population is affected.
Frequently Asked Questions FAQs
Primary hyperhidrosis, (the focus of this webpage), is NOT caused by an underlying medical disease. In addition, primary hyperhidrosis only involves one or two sites of the body, typically starts before 25 years of age, and is bilateral and symmetrical. It occurs only while awake and not during sleep.
Secondary hyperhidrosis is caused by an underlying condition (e.g. metabolic, endocrine, infectious, malignancy, or medication) and occurs while the patient is awake or asleep.
A minimum of six months of visible focal sweating that exceeds normal thermoregulatory needs and includes at least 3 to 4 of the following:
- Involve the palms, soles, armpits, or head and neck area
- Symmetrical bilateral distribution
- Disturbs daily activities
- Occurs at least one time per week
- Onset before 25 years of age
- Lacks symptoms while asleep
- Other family members affected
What treatments are available?
Here are a couple tips that you may find helpful:
- Some people find that avoiding emotional provocations, spicy foods and alcohol are helpful.
- Try to avoid tight clothing, man-made synthetic fabrics and occlusive footwear
- Try masking sweat using underarm liners or dress shields
- For those people who have issues with sweaty feet, frequent sock and shoe changes, leather shoes, absorbent shoe insoles, foot powder and cotton or wool socks may be helpful
 Topical antiperspirants are the first-line therapy for all forms of hyperhidrosis including armpits, palms and soles. These topical agents work by creating a plug in the sweat duct thereby preventing the ability to sweat. A variety of different chemical formulations are available over-the-counter. Aluminum chloride (hexa hydrate) is the most effective topical antiperspirant. This ingredient can be found in various concentrations. The maximum over-the-counter concentration is 12% aluminum chloride. The stronger the preparation the more irritating it may be to the skin. The prescription antiperspirant ( 20% aluminum chloride) under the tradename Drysol, is currently on backorder. Patients may try obtaining an equivalent product online through Amazon.
Topical antiperspirants are the first-line therapy for all forms of hyperhidrosis including armpits, palms and soles. These topical agents work by creating a plug in the sweat duct thereby preventing the ability to sweat. A variety of different chemical formulations are available over-the-counter. Aluminum chloride (hexa hydrate) is the most effective topical antiperspirant. This ingredient can be found in various concentrations. The maximum over-the-counter concentration is 12% aluminum chloride. The stronger the preparation the more irritating it may be to the skin. The prescription antiperspirant ( 20% aluminum chloride) under the tradename Drysol, is currently on backorder. Patients may try obtaining an equivalent product online through Amazon.
General tips on application of antiperspirants:
- Antiperspirants should be applied to dry skin at bedtime. (Using a hair dryer on cool setting to dry the area first before application may be helpful). If aluminum chloride mixes with sweat, it produces hydrochloric acid and is irritating to the skin. That’s why the skin must be bone dry before application. And since we tend not to sweat at bedtime, that is the best time to apply it.
- Antiperspirants need to stay on the skin for 6 to 8 hours before being washed off.
Tips on reducing irritation from antiperspirants:
- When starting out, consider using the strong preparation every other night initially.
- Reduce application to twice-weekly once success is achieved.
- Use the lowest concentration of aluminum chloride possible.
- Apply a moisturizer after application of the antiperspirant.
- Apply a weak preparation of hydrocortisone twice a week maximum.
- Once reduction of sweating is noted ( usually within 1 to 2 weeks of starting a strong antiperspirant), maintenance therapy usually only requires twice a week application.
With regard to safety concerns:
- No evidence exists that links the use of aluminum containing antiperspirants to Alzheimer’s disease
- No clear link exists between the use of aluminum containing antiperspirants and breast cancer
Anticholinergic agents work by inhibiting nerve transmission to the sweat ducts.
Qbrexa ™ was recently approved by the FDA for the treatment of excessive sweating in the armpits.
This product is a topical anticholinergic agent (glycopyrrolate) and comes as a premoistened wipe. The patient is instructed to wipe the armpits at bedtime. It is critical to wash your hands after application in order to prevent accidental exposure to the eyes.
Side effects are infrequent. Potential adverse effects include skin irritation ( far less than antiperspirants), dry mouth, dry eyes, blurry vision, constipation and dizziness.
Anticholinergic agents work by inhibiting nerve transmission to the sweat ducts.
Oral systemic medications are reserved for treatment resistant cases or generalized hyperhidrosis
Anticholinergics are the most commonly used oral medications for hyperhidrosis treatment.
Adverse effects of oral anticholinergics are much higher than seen in topical anticholinergics.
Glycopyrrolate is the most commonly used anticholinergic for hyperhidrosis, as it has the least side effects of its class. The initial dose of glycopyrrolate is usually 1 to 2 mg twice daily. Maximum improvement is typically achieved in one week and requires ongoing daily maintenance therapy.
Adverse effects of glycopyrrolate include dry mouth, blurred vision, dry eyes, overheating, low blood pressure and dizziness, constipation, drowsiness, and urinary retention.
Patients who take glycopyrrolate must be careful on hot days to drink extra water.
We have found that most patients can tolerate low doses of glycopyrrolate with minimal side effects.
Iontopheresis is effective and is considered the primary treatment (after a trial of antiperspirants). It works through use of current transfer from water to skin. The electrodes repel hydrogen ions into sweat ducts thereby reducing sweat secretion.
At home Iontopheresis treatment devices are available for purchase. (e.g. Drionic ™).
Iontopheresis is performed 3 to 4 times per week for 20 to 30 minutes. Approximately 10 to 15 treatments are required to stop sweating and the effects usually last for 2 to 14 weeks. After that, maintenance treatments are performed every 1 to 4 weeks.
Iontopheresis Is about 80% effective.
Therapeutic success and side effects depend on current intensity.
Adverse effects include discomfort, tingling of the hands or feet, redness and transient blisters. Side effects can be lessened with moisturizers, topical steroid cream or a decrease in treatment frequency or intensity.
Addition of aluminum chloride to the water used for Iontopheresis may improve the success.
Botox is a common, safe and effective injectable medication for excess sweating. In our clinic, we inject Botox into the armpits but not to the hands or feet (as this is painful, and there is a risk of muscle weakness).
Most patients with excessive armpit sweating experience excellent results from Botox treatment, lasting approximately 6 to 9 months. sweat reduction is observed within 2 to 4 days and becomes dramatically reduced after approximately two weeks. Most patients with hyperhidrosis require one to two Botox treatments per year.
Approximately 10 to 20 injections are administered in each armpit. Due to the discomfort of the injections, we typically apply topical anesthetic cream 30 minutes prior to injections which renders the procedure virtually painless.
Performing a starch iodine test prior to Botox injections helps map out the extent of the sweat ducts, allowing more precise injections.
Many insurance companies consider Botox treatment for hyperhidrosis necessary only after other topical treatments have failed. Prior authorization from an insurance company is required.
We will hold a credit card deposit until payment from the insurance company is received, at which time the entire amount will be refunded. Usually this is within 30 days.
Contraindications to Botox treatment include peripheral motor neuropathy, neuromuscular disease such as myasthenia gravis, pregnancy, lactation and medications that include cholinesterase inhibitors, and calcium channel blockers.
Microwave thermolysis, Ultrasound therapy, Fractional radiofrequency microneedling, laser procedures and surgical treatment are considered when all other methods have failed. We do not use any of these treatments in our clinic. Further information can be obtained from the International Hyperhidrosis Society.
Sources
- Shiri Nawrocki, Jisan Cha. The etiology, diagnosis, and management of hyperhidrosis: a comprehensive review: etiology and clinical workup. JAAD September 2019
- Shiri Nawrocki, Jisan Cha. The etiology, diagnosis, and management of hyperhidrosis: Therapeutic options. JAAD September 2019